Patient Safety
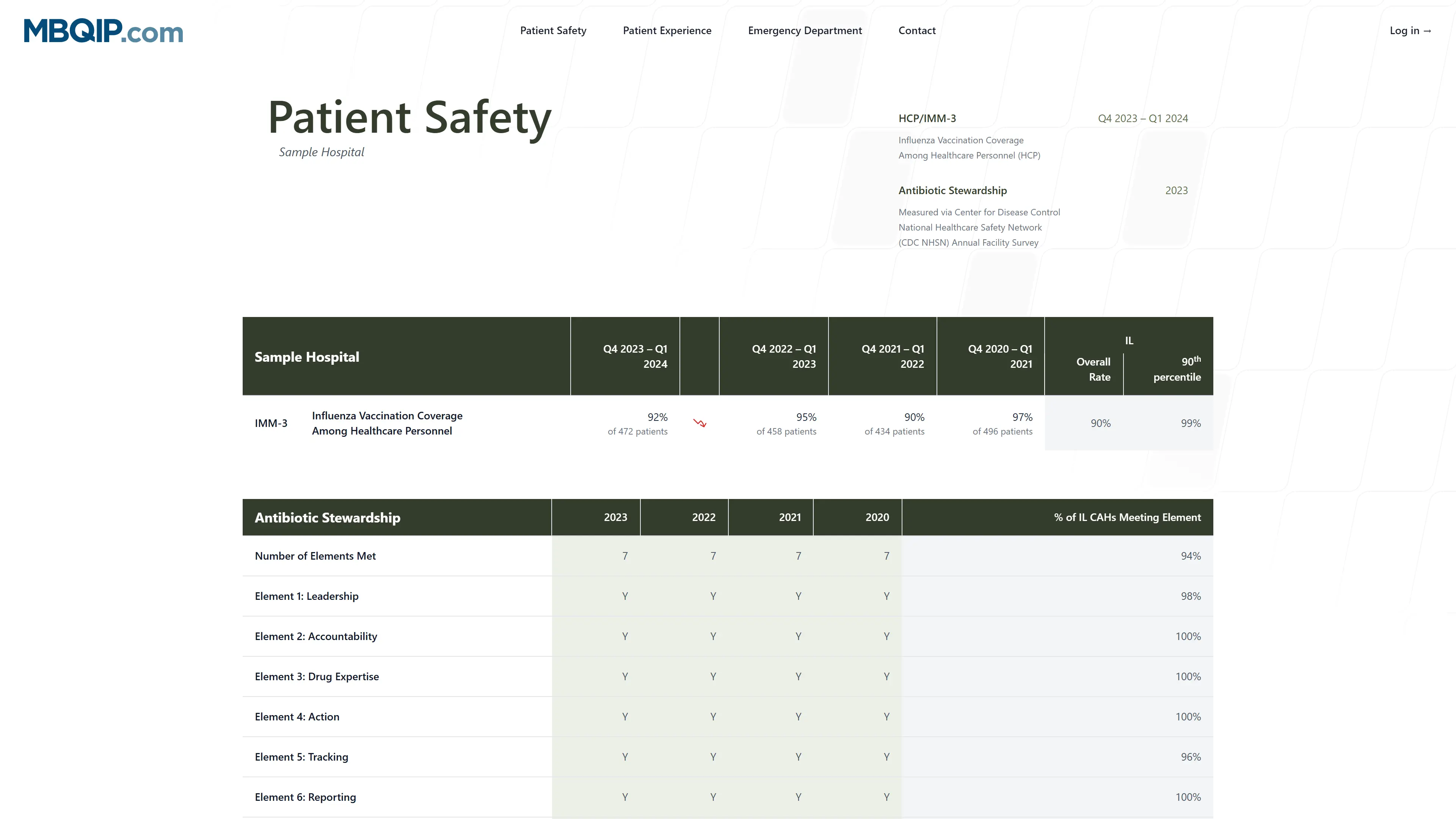
These resources focus on quality improvement related to patient safety and inpatient care. The current MBQIP measures that fall under this domain are HCP/IMM-3 and Antibiotic Stewardship . Safe Use of Opioids (eCQM) will be added as soon as data is received.
View the patient safety report of your hospital
Reports
The MBQIP Patient Safety and Inpatient Care Quality Reports include data from CMS Hospital Compare measures that are relevant for CAHs under the MBQIP domains of patient safety/inpatient care. The reports include data from all CAHs that have signed a MBQIP Memorandum of Understanding (MOU) and have submitted data. Thus, the reports include data from CAHs that have not agreed to publicly report on Hospital Compare, in addition to data from CAHs that don’t have enough cases to be publically reported on Hospital Compare, providing a more complete picture of performance across CAHs nationally.
Using Compairson Data for Patient Safety and Inpatient/Outpatient Measures
MBQIP Patient Safety and Inpatient/Outpatient Care Quality Reports summarize process-based quality measures that evaluate implementation of clinically proven best practices of care. Hospitals should strive to provide these best practices in clinical care to every patient, 100 percent of the time. Each measure includes the following comparison groups:
- all reporting CAHs by state, under the column header CAH State Current Quarter
- all reporting CAHs nationally, under the column header CAH National Current Quarter
- all reporting hospitals nationally (both Prospective Payment System hospitals and CAHs), under the column header All National Current Quarter (unavailable for Antibiotic Stewardship)
Although it can be helpful to understand performance in comparison to those norms, averages represent the middle ground for performance and everyone should strive to achieve at least the 90 th percentile for each measure. For quality improvement purposes, such data benchmarks are more useful than average comparison data.
Measure Information
Encounter Period
October 1, 20XX – March 31, 20XX (Aligns with flu season, for example: October 1, 2023 – March 31, 2024)
Submission Deadline
May 15, 20XX
Data submission deadlines on a federal holiday or weekend (Saturday or Sunday) will
default to the first business day thereafter where applicable.
Measure Description
Influenza Vaccination Coverage among Healthcare Personnel
Measure Rationale
1 in 5 people in the U.S. get influenza each season. Combined with pneumonia, influenza is the 8th leading cause of death, with two-thirds of those attributed to patients hospitalized during the flu season.
Improvement Noted As
Increase in the rate (percent)
Numerator
All HCP personnel who:
- Received vaccination at the facility
- Received vaccination outside of the facility
- Did not receive vaccination due to contraindication
- Did not receive vaccination due to declination
Denominator
All HCP that worked in the facility (part-time or full-time) for at least one day during the encounter period of October 1 – March 31.
Measure Population (Determines the cases to abstract/submit)
All HCP that worked in the facility (part-time or full-time) for at least one day during the encounter period of October 1 – March 31.
Sample Size Requirements
No sampling - report all cases
Calculations
All data reporting is aggregate (whether monthly, once a season, or at a different interval)
Data Source
Administrative Data
Data Collection Approach
Hospital Tracking
Data Elements
Three categories (all with separate denominators) of HCP working in the facility at least one day between 10/1-3/31:
- Employees on payroll
- Licensed independent practitioners
- Students, trainees, and volunteers 18yo+
A fourth optional category is available for reporting other contract personnel. HCP workers who:
- Received vaccination at the facility
- Received vaccination outside of the facility
- Did not receive vaccination due to contraindication
- Did not receive vaccination due to declination
Measure Submission and Reporting Channel
This data is reported annually through the Healthcare Personnel Safety Component of National Healthcare Safety Network (NHSN) website.
Data Available On
MBQIP Data Reports
Other Notes
Each facility in a system needs to be registered separately and HCPs should be counted in the sample population for every facility at which they work. Facilities must complete a monthly reporting plan for each year or data reporting period. All data reporting is aggregated (whether monthly, once a season, or at a different interval).
Learn More
Encounter Period
Calendar Year (January 1, 20XX – December 31, 20XX)
Submission Deadline
March 1, 20XX
Data submission deadlines on a federal holiday or weekend (Saturday or Sunday) will
default to the first business day thereafter where applicable.
Measure Description
Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) Annual Survey
Measure Rationale
Improving antibiotic use in hospitals is imperative to improving patient outcomes, decreasing antibiotic resistance, and reducing healthcare costs. According to the Centers for Disease Control and Prevention (CDC), 20-50 percent of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate, which leads to serious side effects such as adverse drug reactions and Clostridium difficile infection. Overexposure to antibiotics also contributes to antibiotic resistance, making antibiotics less effective.
In 2014, CDC released the “Core Elements of Hospital Antibiotic Stewardship Programs,” which identifies key structural and functional aspects of effective programs and elements designed to be flexible enough to be feasible in hospitals of any size.
Improvement Noted As
Increase in the number of core elements met
Measure Population
NA – This measure uses administrative data and not claims to determine the measure’s denominator population.
Sample Size Requirements
No sampling – report all information as requested
Data Collection Approach
Hospital tracking
Data Elements
Questions as answered on the Patient Safety Component Annual Hospital Survey inform whether the hospitals have successfully implemented the following core elements of antibiotic stewardship:
- Leadership
- Accountability
- Drug Expertise
- Action
- Tracking
- Reporting
- Education
Measure Submission and Reporting Channel
National Healthcare Safety Network (NHSN) website
Learn More
Encounter Period
Calendar Year (January 1, 20XX – December 31, 20XX)
Submission Deadline
February 28, 20XX
Data submission deadlines on a federal holiday or weekend (Saturday or Sunday) will
default to the first business day thereafter.
Measure Rationale
Unintentional opioid overdose fatalities have become an epidemic and major public health concern in the United States. Concurrent prescriptions of opioids, or opioids and benzodiazepines, places patients at a greater risk of unintentional overdose due to increased risk of respiratory depression. Patients who have multiple opioid prescriptions have an increased risk for overdose, and rates of fatal overdose are ten (10) times higher in patients who are co-dispensed opioid analgesics and benzodiazepines than opioids alone. A measure that calculates the proportion of patients with two or more opioids or opioids and benzodiazepines concurrently has the potential to reduce preventable mortality and reduce costs associated with adverse events related to opioids.
Measure Program Alignment
Safe Use of Opioids is a current measure of the Medicare Promoting Interoperability (PI) Program. Critical access hospitals must meet PI Program requirements on an annual basis to avoid a downward payment. One of the program requirements is submission of electronic clinical quality measures (eCQM) data from certified electronic health record technology (CEHRT). Calendar year (CY) 2023 eCQM reporting requirements for PI include data reflecting all four quarters of CY 2023 for:
- Three self-selected measures of the thirteen available eCQMs for each quarter
- One required measure: Safe Use of Opioid Measure
Improvement Noted As
Decrease in the rate
Numerator
Inpatient hospitalizations where the patient is prescribed or continuing to take two or more opioids or an opioid and benzodiazepine at discharge.
Denominator
Inpatient hospitalizations (inpatient stay less than or equal to 120 days) that end during the measurement period, where the patient is 18 years of age and older at the start of the encounter and prescribed one or more new or continuing opioid or benzodiazepine at discharge.
Exclusions
Inpatient hospitalizations where patients have cancer that begins prior to or during the encounter or are ordered or are receiving palliative or hospice care (including comfort measures, terminal care, and dying care) during the hospitalization or in an emergency department encounter for observation stay immediately prior to hospitalization, patients discharged to another inpatient care facility, and patients who expire during the inpatient stay.
Measure Population (Determines the cases to abstract/submit)
Inpatient hospitalizations (inpatient stay less than or equal to 120 days) that end during the measurement period, where the patient is 18 years of age and older at the start of the encounter and prescribed one or more new or continuing opioid or benzodiazepine at discharge.
Sample Size Requirements
No sampling – report all patients that meet data elements
Calculations
Numerator divided by Denominator
Data Source
Certified electronic health record technology (CEHRT)
Data Collection Approach
Electronic Extraction from EHRs via Quality Reporting Document Architecture (QRDA) Category I File
Measure Submission and Reporting Channel
Annually, via Hospital Quality Reporting (HQR) Secure Portal as any combination of: QRDA Category I File, zero denominator declarations and/or case threshold exemptions (<=5 cases in the reporting quarter)
