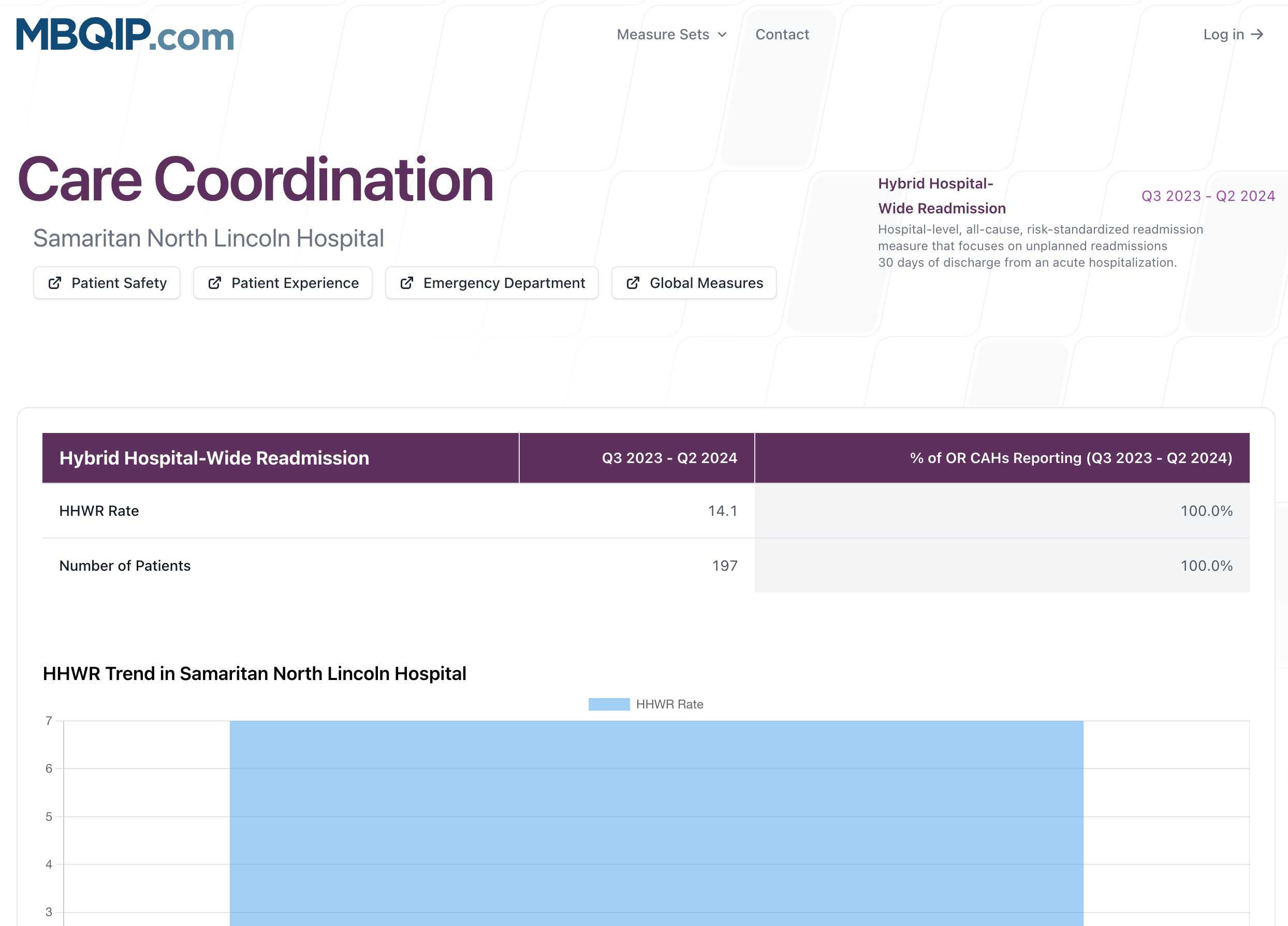
Care Coordination
These resources focus on quality improvement related to unplanned hospital readmissions and the social drivers that influence patient outcomes. The current CMS IQR measures that fall under this domain are the Hybrid Hospital‑Wide Readmission (HWR) rate.
View the care transitions report of your hospital
Reports
The Care Transitions combine CMS‑calculated readmission results—which link electronic health record data with claims—with hospital‑reported data on screening for food insecurity, housing instability, transportation needs, utility difficulties, and interpersonal safety. Reports include every short‑term acute‑care hospital that submits patient‑level files, giving a comprehensive view of nationwide performance.
Using Comparison Data for Readmission
Care Transitions summarize both outcome‑based and process‑based measures that highlight opportunities to improve discharge planning, care coordination, and connections to community resources. Each measure includes the following comparison groups:
- All reporting hospitals in your state (column State Current Quarter)
- All reporting hospitals nationally (column National Current Quarter)
- Top‑decile performance benchmark (column 90th Percentile)
Averages show the middle ground, but hospitals should strive to meet or exceed the 90th‑percentile benchmark for each measure to meaningfully reduce avoidable readmissions and address unmet social needs.
Measure Information
Encounter Period
July 1, 20XX - June 30, 20XX
Submission Deadline
September 30, 20XX ; Data submission deadlines on a federal holiday or weekend (Saturday or Sunday) will default to the first business day thereafter in this document where applicable.
Measure Description
Hospital-level, all-cause, risk-standardized readmission measure that focuses on unplanned readmissions 30 days of discharge from an acute hospitalization.
Hybrid measures differ from the claims-only measures in that they merge electronic health record (EHR) data elements with claims-data to calculate the risk-standardized readmission rate. The Hybrid HWR was developed to address complex and critical aspects of care that cannot be derived through claims data alone. The Hybrid HWR uses EHR data including clinical variables and linking elements for each patient:
- Clinical variables (13): Heart Rate, Systolic Blood Pressure, Respiratory Rate, Temperature, Oxygen Saturation, Weight, Hematocrit, White Blood Cell Count, Potassium, Sodium, Bicarbonate, Creatinine, Glucose
- Linking elements (5): CMS Certification Number (CCN), National Provider Identifier (NPI) for MA patients, Medicare beneficiary Identifier (MBI), Inpatient Admission Date, and Discharge date.
It is recommended hospitals only report the FIRST resulted value for EACH core clinical data element collected in the appropriate timeframe, if available. Hospitals may also choose to report ALL values on an encounter during their entire admission; however, only the first resulted values are utilized in the logic for measure calculation.
Measure Rationale
Returning to the hospital for unplanned care disrupts patients’ lives, increases risk of harmful events like healthcare-associated infections, and results in higher costs absorbed by the health care system. High readmission rates of patients with clinically manageable conditions in primary care settings, such as diabetes and bronchial asthma, may identify quality-of-care problems in hospital settings. A measure of readmissions encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions and costs.
Measure Program Alignment
CMS Inpatient Quality Reporting (IQR) program measure.
Improvement Noted As
No actual measure score will be generated by hospitals. Instead, hospitals will report the data values for each of the core clinical data elements for all encounters in the Initial Population. These core clinical data elements will be linked to administrative claims data and used by CMS to calculate results for the Hybrid HWR measure.
Numerator
If a patient has more than one unplanned admission (for any reason) within 30 days after discharge from the index admission, only one is counted as a readmission. The measure looks for a dichotomous yes or no outcome of whether each admitted patient has an unplanned readmission within 30 days. However, if the first readmission after discharge is considered planned, any subsequent unplanned readmission is not counted as an outcome for that index admission because the unplanned readmission could be related to care provided during the intervening planned readmission rather than during the index admission.
Denominator
- Enrolled in Medicare FFS Part A for the 12 months prior to the date of admission and during the index admission or enrolled in Medicare Advantage;
- Aged 65 or over;
- Discharged alive from a non-federal short-term acute care hospital;
- Not transferred to another acute care facility
Exclusions
The measure excludes index admissions for patients:
- Admitted to Prospective Payment System (PPS)-exempt cancer hospitals;
- Without at least 30 days post-discharge enrollment in Medicare FFS;
- Discharged against medical advice (AMA);
- Admitted for primary psychiatric diagnoses;
- Admitted for rehabilitation; or
- Admitted for medical treatment of cancer
Measure Population (Determines the cases to abstract/submit)
All Medicare FFS and MA hospitalizations for patients aged 65 and older at the start of an inpatient admission, where the length of stay is less than 365 days, and the hospitalization ends during the measurement period.
The initial population includes patients with inpatient hospitalizations and patients from Acute Hospital Care at Home programs, who are treated and billed as inpatients but receive care in their home.
NOTE: All Medicare FFS and MA hospitalizations meeting the above criteria should be included, regardless of whether Medicare FFS/MA is the primary, secondary, or tertiary payer.
Sample Size Requirements
No sampling – report on all information requested in denominator and numerator.
Data Collection Approach
Hybrid – chart extraction of electronic clinical data and administrative claims data.
Data Elements
Core Clinical Data Elements (13)
- Heart Rate
- Systolic Blood Pressure
- Respiratory Rate
- Temperature
- Oxygen Saturation
- Weight
- Hematocrit
- White Blood Cell Count
- Potassium
- Sodium
- Bicarbonate
- Creatinine
- Glucose
For each encounter, please also submit the following Linking Variable:
- CMS Certification Number (CCN)
- National Provider Identifier (NPI) for MA patients
- Medicare Beneficiary Identifier (MBI)
- Inpatient Admission Date
- Discharge Date
Measure Submission and Reporting Channel
Annual-Hospital Quality Reporting (HQR) via patient-level file in QRDA I format
